The Distant Metabolic Gift vs. Low-Fat Federal Dietary Guidelines
[Revised from original May 16th post]
Mostly stuck in the pandemic, curious about Covid-19, social distancing, and lockdowns, plus regulation of testing, masks, and treatments. Best maybe not to watch evening news (better described as “evening narratives”), with Administration, Governors, and commentators battle over cases, hospitalizations, and policies. But dozens of thoughtful articles and studies are available from reputable publications and organizations, with research on disease, microbes, and epidemics.
(May 16th–nearly two months ago!–company still waiting for FDA approval to test): Antibodies the news today: Coronavirus Breakthrough? Possible Antibody Cocktail May Lead To COVID-19 Cure, Doctor Says (CBS New York, May 15, 2020).
Sorrento CEO Dr. Henry Ji says its antibody, STI-1499, has provided 100% inhibition of the SARS-COV-2 virus in pre-clinical tests. Dr. Ji went so far as to call it a cure.
Pandemic and lockdown events have been politicized by media reports and press conferences. Plenty of blame to go around, but people seem to fall on the lockdown longer and harder side or the end the lockdown side, and on side of too little too late government action caused the pandemic, or the too much government regulation and delay did.
But even with the worldwide pandemic, lockdowns, and economic collapse seeming the biggest stories possible, there is a deeper reality lurking in the background. The pandemic has been a fast-forward event, pulling the next few years of disease and mortality into the last few months. Economic historians may come to see the story as about the “metabolically gifted,” those better suited for pre-industrial times. When food was scarce and famines stalked the world, adding weight quickly in summer and fall was often key to surviving winter.
Today with food abundance, this gift becomes a metabolic syndrome or disorder. And this metabolic syndrome, insulin resistance, puts tens of millions of Americans at higher risk of various dangerous medical conditions, as well as much higher risk for severe Covid-19 symptoms.
Government nutritional policies and programs are at the center of this expanding public health disaster. Public health officials were misled by weak research fifty years ago and institutional inertia plus food industry pressure have locked in policies ever since. It is a strange history and the diet guidelines battle continues today. The story shouldn’t surprise economists and historians who know regulatory capture theory. Economists make the case that federal regulatory agencies serve and protect special interests more than the general public (education, transportation, finance, defense, energy, and housing, for example).
Why Federal Nutritional Guidelines Matter for Covid-19
Covid-19 spreads rapidly and widely because it doesn’t make most people very sick. Most are asymptomatic. At least 50% don’t have symptoms and for most of the rest symptoms are mild. But “asymptomatic” is complicated and the actually asymptomatic may be less than 50%: The Term ‘Asymptomatic’ Is More Complicated Than It Seems When It Comes To Coronavirus Infections (Forbes, May 16, 2020)
Estimates of the percentage of Covid-19 infections that progress to serious or critical vary. WHO says 20%, so one in five. Worldometers has serious or critical at 2% (2,529,892 mild and 44,810 serious/critical as of May 16), but that’s because some testing positive are okay now but will get worse in coming days or weeks. Estimates of how many will have serious symptoms is unknown due to inadequate testing for Covid-19 and for antibodies found in those already recovered. Eventually we will have better estimates from more testing.
Focus then should be on those serious and critical cases, and nearly all have pre-existing conditions, mainly high blood pressure, cardiovascular disease, and diabetes.
Most who die from Covid-19 (or from misguided treatment) have co-morbidities like hypertension and diabetes. “The most common co-morbidities were hypertension, obesity, and diabetes” reports this April 22, 2020 JAMA article surveying 5,700 Covid-19 patients in New York City area. A March report from Italy claimed: 99% of Those Who Died From Virus Had Other Illness, Italy Says.
But countries count Covid-19 in different ways so cross-country comparisons are difficult.
Another article looks at obesity, especially for those under 60:
As part of the COVID-19 response team at O’Connor Hospital in San Jose, Calif., Nivedita Lakhera wasn’t prepared to see her intensive care unit filled with so many young patients. Many of those patients had no medical condition other than obesity. …
Age, particularly those over 65, as well as having a compromised immune system are still major risk factors for being hospitalized with, and dying from, COVID-19. But some doctors say that some of their sickest patients are those under 60 who are obese.
COVID-19 is hitting some patients with obesity particularly hard (Science News, April 22)
According the the Center for Disease Control (CDC), close to half of adults the U.S. fall into the obese category (42.4% for 2017-18), with nearly 9.2% considered severely obese. The CDC also reports 34 million American have diabetes and 88 million have pre-diabetes (National Diabetes Statistics Report, 2020). Also, blacks and hispanics have higher rates of diabetes helping explain news reports of much higher mortality from Covid-19.
Diabetes and obesity are linked, but how they are linked is a subject of intense research and debate among doctors and epidemiologists. The common narrative is that people gain weight because they eat too much and don’t exercise enough. Count calories say the public health authorities, eat a (government-defined) balanced diet, and get plenty of exercise!
Turns out this advice is dead wrong for the metabolically gifted. Their systems are too efficient for the modern world. The low-fat/

high-carb Food Pyramid (now Food Plate) that public health officials have pushed since the 1970s overloads their insulin resistant metabolisms.
Quick overview by: Dr Peter Brukner and LCHF, SO YOU WANT TO KNOW ABOUT LOW CARB, HIGH FAT (LCHF):
Up until about 30 years ago most Western societies ate a diet containing plenty of saturated fat in the form of butter, milk, cream and fatty meats. Then on the basis of some flimsy research, the U.S initially, followed by other countries, decided to adopt a low fat diet. It seemed to make sense and was an easy concept to sell – fatty foods lead to fat people with fatty arteries leading to cardiovascular disease.
The only problem is that is hasn’t worked! In the last thirty years coinciding with the switch to a low fat diet, the incidence of obesity and Type 2 diabetes has steadily increased.
The reason for this is that the cause of obesity and diabetes is probably excess carbohydrates rather than excess fat. The low fat mantra and its associated food pyramid has resulted in increased carbohydrate intake in the form of grains, cereals, bread, pasta, rice etc. In addition, in many “low fat” foods when the fat was removed, the manufacturers replace it with carbs such as high fructose corn syrup to improve the taste. …
Detour Back to Pandemic, then to Nutrition Debate
Much blame for the pandemic in the U.S. has been directed at the CDC and FDA (Food and Drug Administration) for their policies and edicts blocking and delaying state, university, and private Covid-19 testing and treatments. That’s important and many articles report what happened. This one from March: Coronavirus testing delays caused by red tape, bureaucracy and scorn for private companies ( NBC News, March 18). New York Times story. And from April: The Monumental Failure of the CDC (AIER, April 11, 2020)
FDA and CDC regulations still derail testing and treatment development. See: The FDA has shut down a Bill Gates-backed coronavirus testing program (DigitalTrends, May 15, 2020.
However, there is a bigger, deeper story of federal nutritional policies as the source of America’s obesity and diabetes epidemic, creating today’s main Covid-19 risks.
A growing network of medical researchers make the case that CDC, FDA, and USDA misguided nutrition policies, backed by the food industry, created the upsurge of obesity and diabetes since the 1980s. These federal agencies continue to promote and protect their nutrition policies and, with food industry help, fight against alternative dietary guidelines that could reverse obesity and diabetes.
Another grand conspiracy theory! And with enough room for blame and condemnation for food corporations and associations as well as state and federal government agencies, plus entrenched university nutrition departments. Is a low-fat diet with lots of fruits, vegetables, and grains the best? Or was the diet most Americans consumed until the 1980s better, one with more calories from fat and fewer from carbohydrates and sugar?
For a quick overview of the story see various books, articles, and videos (videos reference extensive peer-reviewed research):
• Why Does the Federal Government Issue Damaging Dietary Guidelines? Lessons from Thomas Jefferson to Today (Cato, July 10, 2018)
* Sugar and the State (essays, discussion) (Cato Unbound, January, 2017)
• Nina Teicholz – ‘The Real Food Politics’ [author of The Big Fat Surprise]
And more history of this political nutritional story with an “Empire Strikes Back” theme in this YouTube video:
• Dr. Jay Wortman – ‘Undoing Atkins: A Cautionary Tale’
About Dr. Jay Wortman.
Two views: Blame government or blame food industry?:
• Government dietary guidelines are plain wrong: Avoid carbs, not fat (The Hill, November 29, 2018)
* Dietary guidelines: Blame Big Food, not government, for unhealthy eating (The Hill, December 20, 2018)
The pre-existing conditions so deadly when Covid-19 strikes can be reversed according to doctors who have reversed diabetes in thousands of patients and enabled tens of thousands more to return to weights normal for their body type (exiting obesity). There are many chapters to the nutritional story, from biochemical individuality, to our unique microbiomes, to the way each person’s metabolism responds to macronutrients.
Obesity and diabetes will overwhelm health care systems in the coming decades, as well as putting millions at high risk for Covid-19 (as well as influenza) today.
Federal nutritional guidelines, promoted at all levels of American society, including schools (and school “free” student lunch programs) are a source of the problem. Medical doctors have been prosecuted for recommending recommending low-carb diets. Nutritionist get warned by their associations they could lose their license. (references in videos).
Over the last few years though, the effectiveness of cutting sugar and carbohydrate consumption in reversing diabetes have converted more and more doctors to the reality of low-carbs (and/or no sugar) for those with metabolic syndrome (what I’ve called the “metabolic gift” for pre-industrial, food-scarce times).
Just two weeks ago I was 5% above the obesity line, according to my Eufy scale. Then I started watching various Low Carb Down Under YouTube videos (beginning with the Nina Tiecholz video above).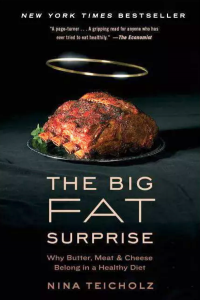
Viewpoints differ: some speakers make the case for low-carb and high animal fats, others focus on the danger of sugar, others fructose, others note that genetic differences allow high starch to work for some and all-fat for other populations. Most say to stay away from processed foods and vegetable (or seed) oils. Other doctors and nutritionists recommend intermittent fasting. Dr. Jason Fung says yes to fasting (video), Mayo clinic 1-minute video says no on fasting. Another Mayo video, maybe some benefits, be careful.
But watching the videos led me to alter my diet. Starting two weeks ago I stopped eating cookies, ice cream bars, candies, and consumed more meat, milk, cheese, eggs, smoked salmon, and blueberries. I’ve been eating just one meal a day and for some reason don’t get hungry. I’m exercising more, walking and jogging an average of 15,000 steps a day (according to Fitbit). I’ve had a few chocolate chips cookies, and they were great, but I didn’t crave any more. No potato chips.
Today, May 16, my BMI and body fat percentages are still high: 27.6% and 28.4%, (under 25% is recommended). Two weeks ago, on May 3, both measures were higher: BMI was 29.3% and body fat was 30.3%. I weighed 228.3 on May 3 and this morning, two weeks later, weigh 215.3. Maybe I could write my own books with a title like “Don’t Diet: Just Watch Low Carb Down Under Videos.”
I’m healthy as far as I know, but my father was diagnosed with type 2 diabetes at about my age. I remembered he had been slowly gaining weight since the 1980s, and noticed in the mirror and on the scale that I’d been gaining weight too. When I hit 230 I started walking more and for a month weighed myself each morning, alway staying around 228.
I don’t want to suffer from type 2 diabetes as my father did. And I hope tens of millions of Americans can step back from obesity and diabetes. Further research and discussion of diet and nutrition, and a push-back against misguided federal nutrition guidelines, will save billions of health care dollars and help millions challenged by the distant “metabolic gift” that in the modern world has become a syndrome.
